Our approach
How do the colorectal cancer models work?
We use individual-based microsimulation models to simulate colorectal cancer screening, cancer diagnosis and treatment, and costs in both North Carolina and Oregon. The simulated individuals age and experience changes in cancer status over time, and their individual-level and population-level outcomes are tracked for various screening interventions and health policy changes tested.
The models integrate the best available data on the development and progression of colorectal polyps and cancer, demographic characteristics of the state residents, baseline compliance with recommended screening and surveillance, screening test characteristics (i.e. sensitivity and specificity of colonoscopy and stool tests), and more input parameters. Model outputs include receipt of cancer screening, development of cancer, cancer deaths, years of life lost due to cancer, and costs of cancer screening and treatment. The outputs are measured for each intervention or policy scenario as compared to the status quo "screening as usual" scenario (i.e. what is expected to occur in the absence of intervention).
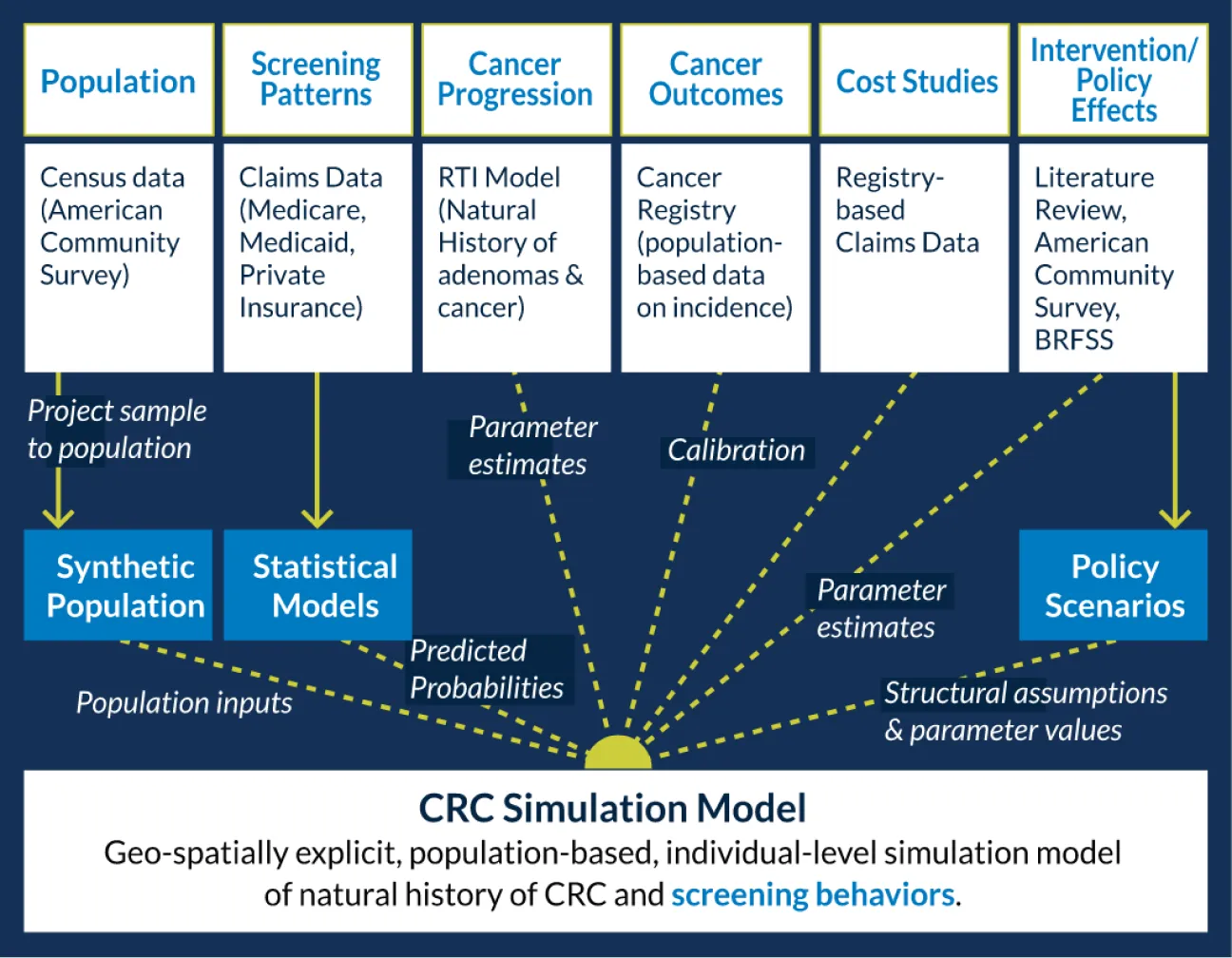
The model was developed by members of our team at the University of North Carolina at Chapel Hill, North Carolina State University, and Oregon Health & Science University using AnyLogic simulation software.
Additional details about our CRC PopSim model can be found in the technical supplement, available here: https://crcsim.web.unc.edu.
What information can the models produce?
Our population-level simulation models have many capabilities, including, but not limited to:
- Integrates multiple data sources to evaluate the effects of specific policies and interventions
- Simulates the behaviors, experiences, and outcomes of realistic and diverse populations
- Accounts for local nuances and differential impact of interventions in different contexts
- Quantifies the expected uptake and health and economic impact of specific interventions and policies in specific contexts, settings and sub-populations
- Forecasts outcomes over long time periods, with attention to uncertainty
- Models combinations of interventions to understand potential interacting, synergistic, or ceiling effects when attempting to encourage specific health behaviors within a population
- Assesses the full continuum of cancer care outcomes, such as: quality adjusted life years (QALYs),cost per person screened, cost per cancer case averted, and cost per QALY gained

Using the models to help make decisions
We designed this interactive, web-based tool to allow users to understand how interventions and health policies are anticipated to affect colorectal cancer screening and outcomes in their populations of interest. Users can vary the input parameters and explore how the expected outcomes will change as a result.
Although the model is currently only developed for North Carolina and Oregon, stakeholders in other states can still modify the input parameters to most closely resemble their local populations. We hope that this tool will allow stakeholders to make informed decisions about how to improve colorectal cancer screening locally, paying particular attention to the opportunities to reduce morbidity and mortality associated with colorectal cancer in the population at large and within underserved communities.

Current applications
We have used the Cancer Control PopSim model designed for colorectal cancer for the following purposes:
- To estimate the impact of evidence-based interventions and health insurance changes on colorectal cancer screening and outcomes
- To assess what it would take to achieve colorectal cancer screening targets
- To estimate the cost-effectiveness of particular strategies in improving colorectal cancer screening and outcomes compared to usual care
- To identify strategies for reducing existing disparities in colorectal cancer screening rates and outcomes
Please see our publications for more information on these activities.
