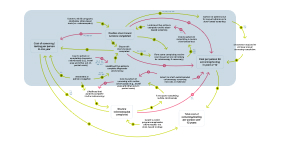
What impacts the cost of stool-based screening?
The cost of screening to patients is an important consideration. Programs emphasizing stool-based tests see more completed screens, increasing the likelihood of positive results that require follow-up diagnostic colonoscopies. Even if the CRCCP covers the colonoscopy, patients incur costs such as bowel preparation and medication.39, 163, 168, 427 Higher procedure costs reduce the likelihood of patients completing diagnostic colonoscopies.
Investing in patient navigation services increases the likelihood of diagnostic colonoscopy completion,88, 89, 434, 456 but requires additional investment, raising the cost per person for one year.213 A balancing loop (B1) exists because patients also accrue costs from time spent completing screening. Time costs, especially for diagnostic colonoscopies following positive stool tests,162, 163, 166 reduce the likelihood of routine screening completion.164
Cited references for this diagram
The largest time cost was related to bowel preparation and undergoing the colonoscopy procedure; therefore, potentially, noninvasive fecal-based tests could result in lower burden in terms of time lost. Fecal tests, though, require much more frequent screening than colonoscopy and, therefore, may not effectively save much money over the long term.
Hoover S, Subramanian S, Tangka FKL, Cole-Beebe M, Sun A, Kramer CL, Pacillio G. Patients and caregivers costs for colonoscopy-based colorectal cancer screening: Experience of low-income individuals undergoing free colonoscopies. Eval Program Plann. 2017 Jun;62:81-86. doi: 10.1016/j.evalprogplan.2017.01.002. Epub 2017 Jan 7. PMID: 28153341; PMCID: PMC5847315.
In this study, based on retrospective self-reports, patients spent, on average, 23.7 h preparing for, traveling for and having a colonoscopy, and an additional 5.1 h, on average, recovering from the colonoscopy. This translated into a total cost of $335.95 for the patient in lost time and $79.03 for the caregiver. In addition, an estimated $17.46 was incurred in travel and other costs. Even when colonoscopy is provided free of charge to the patient, additional costs may be incurred which could be a significant barrier for low income individuals to receive CRC screening.
Hoover S, Subramanian S, Tangka FKL, Cole-Beebe M, Sun A, Kramer CL, Pacillio G. Patients and caregivers costs for colonoscopy-based colorectal cancer screening: Experience of low-income individuals undergoing free colonoscopies. Eval Program Plann. 2017 Jun;62:81-86. doi: 10.1016/j.evalprogplan.2017.01.002. Epub 2017 Jan 7. PMID: 28153341; PMCID: PMC5847315.
In total, patients needed 28.8 h to undergo the colonoscopy screening, resulting in an indirect average cost of $335.95, while it cost the caregiver $79.03.
Hoover S, Subramanian S, Tangka FKL, Cole-Beebe M, Sun A, Kramer CL, Pacillio G. Patients and caregivers costs for colonoscopy-based colorectal cancer screening: Experience of low-income individuals undergoing free colonoscopies. Eval Program Plann. 2017 Jun;62:81-86. doi: 10.1016/j.evalprogplan.2017.01.002. Epub 2017 Jan 7. PMID: 28153341; PMCID: PMC5847315.
Many studies have documented barriers to cancer screenings in general and CRC screenings in particular. The barriers include low levels of education, language or communication challenges, low socioeconomic status, and lack of insurance coverage (Gimeno Garcia, 2012; Heitman, Au, Manns, McGregor, & Hilsden, 2008; Subramanian, Klosterman, Amonkar, & Hunt, 2004). Cost has also been cited as a barrier (Jones, Devers, Kuzel, & Woolf, 2010; Klabunde et al., 2005).
Hoover S, Subramanian S, Tangka FKL, Cole-Beebe M, Sun A, Kramer CL, Pacillio G. Patients and caregivers costs for colonoscopy-based colorectal cancer screening: Experience of low-income individuals undergoing free colonoscopies. Eval Program Plann. 2017 Jun;62:81-86. doi: 10.1016/j.evalprogplan.2017.01.002. Epub 2017 Jan 7. PMID: 28153341; PMCID: PMC5847315.
Although the authors found that direct clinical costs were higher for colonoscopy-only screening programs than for FOBT/FIT-only programs, nonclinical costs did not vary by screening test type, suggesting that these programs have substantial fixed costs.
Joseph DA, DeGroff A. The CDC Colorectal Cancer Control Program, 2009-2015. Prev Chronic Dis. 2019 Dec 5;16:E159. doi: 10.5888/pcd16.190336. PMID: 31808418; PMCID: PMC6896829.
Implementation of patient navigation and community health workers remained flat over time, likely due, in part, to the need for ongoing funding for staff.
Maxwell AE, DeGroff A, Hohl SD, Sharma KP, Sun J, Escoffery C, Hannon PA. Evaluating Uptake of Evidence-Based Interventions in 355 Clinics Partnering With the Colorectal Cancer Control Program, 2015-2018. Prev Chronic Dis. 2022 May 19;19:E26. doi: 10.5888/pcd19.210258. PMID: 35588522; PMCID: PMC9165474.
Based on a single screening cycle for FOBT, screening with FOBT, including colonoscopy follow-up, was less costly than colonoscopy, both per person and per program.
Seeff LC, DeGroff A, Joseph DA, Royalty J, Tangka FK, Nadel MR, Plescia M. Moving forward: using the experience of the CDCs' Colorectal Cancer Screening Demonstration Program to guide future colorectal cancer programming efforts. Cancer. 2013 Aug 1;119 Suppl 15:2940-6. doi: 10.1002/cncr.28155. PMID: 23868488.
Specifically, highly reported patient barriers among BCC and CRC PNs included lack of: knowledge about cancer; knowledge about cancer screening procedures; knowledge about the benefit of screening; motivation to get screened; transportation; and health insurance.
Barrington WE, DeGroff A, Melillo S, Vu T, Cole A, Escoffery C, Askelson N, Seegmiller L, Gonzalez SK, Hannon P. Patient navigator reported patient barriers and delivered activities in two large federally-funded cancer screening programs. Prev Med. 2019 Dec;129S:105858. doi: 10.1016/j.ypmed.2019.105858. Epub 2019 Oct 22. PMID: 31647956; PMCID: PMC7055651.
The clinical cost of colonoscopy was almost 5 times the cost of FOBT/FIT per person when screening and diagnostic follow-up tests were included. Therefore, programs that use colonoscopy will only be able to screen about one-fifth the number of people that FOBT/FIT programs can for the same level of funding in the initial years of the program. This cost would only affect the number of people screened in the short term because colonoscopy is recommended every 10 years for those at average risk and with normal results, whereas FOBT/FIT is recommended to be performed annually. The clinical costs over a 10-year period for colonoscopy and FOBT/FIT may not be substantially different.
Subramanian S, Tangka FKL, Hoover S, Cole-Beebe M, Joseph D, DeGroff A. Comparison of Program Resources Required for Colonoscopy and Fecal Screening: Findings From 5 Years of the Colorectal Cancer Control Program. Prev Chronic Dis. 2019 Apr 25;16:E50. doi: 10.5888/pcd16.180338. PMID: 31022371; PMCID: PMC6513474.
Systematic reviews have identified barriers to CRC screening including low levels of education, language or communication issues, low socioeconomic status, lack of insurance coverage, and general attitudes towards prevention (for example, smokers are less likely to seek screening) (Gimeno Garcia, 2012; Subramanian et al., 2004).
Tangka FKL, Subramanian S, Hoover S, Royalty J, Joseph K, DeGroff A, Joseph D, Chattopadhyay S. Costs of promoting cancer screening: Evidence from CDC's Colorectal Cancer Control Program (CRCCP). Eval Program Plann. 2017 Jun;62:67-72. doi: 10.1016/j.evalprogplan.2016.12.008. Epub 2016 Dec 12. PMID: 27989647; PMCID: PMC5840873.
Grantees in areas with a screening prevalence of 69.6% or higher allocated the smallest proportion of their screening promotion funds to outreach and education compared with grantees in areas with a screening prevalence of 69.5% or lower. The priority for grantees in areas with higher screening prevalence is navigating the patients along the screening continuum to ensure adherence with recommended screening, diagnostic follow-up, and referral for treatment recommendations; thus, these grantees spent more resources on patient navigation.
Tangka FKL, Subramanian S, Hoover S, Cole-Beebe M, DeGroff A, Joseph D, Chattopadhyay S. Expenditures on Screening Promotion Activities in CDC's Colorectal Cancer Control Program, 2009-2014. Prev Chronic Dis. 2019 Jun 6;16:E72. doi: 10.5888/pcd16.180337. PMID: 31172915; PMCID: PMC6583814.
The patient navigator identified barriers (N=148) to patients being screened for colorectal cancer or other cancers. The largest categories of barriers identified included financial or insurance issues (30.4%, 45/148); psychosocial issues, such as fear of the test and fear of test outcome (23.6%; 35/148); and transportation (23.6%; 35/148).
Tangka FKL, Subramanian S, Hoover S, Cariou C, Creighton B, Hobbs L, Marzano A, Marcotte A, Norton DD, Kelly-Flis P, Leypoldt M, Larkins T, Poole M, Boehm J. Improving the efficiency of integrated cancer screening delivery across multiple cancers: case studies from Idaho, Rhode Island, and Nebraska. Implement Sci Commun. 2022 Dec 16;3(1):133. doi: 10.1186/s43058-022-00381-4. PMID: 36527147; PMCID: PMC9756516.
However, some recent studies with more rigorous study designs have evaluated the effectiveness of PN in increasing CRC screening and found PN effective in addressing individual and system barriers to CRC screening faced by low-income, underserved populations,[[14–16]] improving screening quality, as well as follow-up and diagnostic care, for patients with abnormalities.[[17,18]]
Escoffery C, Fernandez ME, Vernon SW, Liang S, Maxwell AE, Allen JD, Dwyer A, Hannon PA, Kohn M, DeGroff A. Patient Navigation in a Colorectal Cancer Screening Program. J Public Health Manag Pract. 2015 Sep-Oct;21(5):433-40. doi: 10.1097/PHH.0000000000000132. PMID: 25140407; PMCID: PMC4618371.
The high percentage of grantees supporting navigators who are conducting tracking and follow-up activities for both FOBT and colonoscopy is promising, given that these efforts are critical to supporting screening and diagnostic test adherence.
Escoffery C, Fernandez ME, Vernon SW, Liang S, Maxwell AE, Allen JD, Dwyer A, Hannon PA, Kohn M, DeGroff A. Patient Navigation in a Colorectal Cancer Screening Program. J Public Health Manag Pract. 2015 Sep-Oct;21(5):433-40. doi: 10.1097/PHH.0000000000000132. PMID: 25140407; PMCID: PMC4618371.