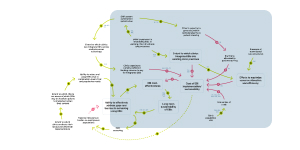
How can clinics maximize resources allocation and efficiency
The automation/optimization of EHR systems requires a high initial investment,212, 356 but embedding EBIs into existing clinic structures and processes increases the extent to which clinics integrate EBIs.212, 251 Coordinating EBIs with existing clinic practices boosts efficiency,271 reducing the cost of EBI implementation and sustainability.175
Team-based care structures also enhance efficiency.246 Economies of scale play a role in reducing costs; larger clinic population sizes298, 386, 404 lower the cost per patient of EBI implementation.60, 382, 387, 403, 424, 441
Cited references for this diagram
Program planners should carefully consider the potential reach and infrastructure costs of direct CRC screening services given available sources of funding, the size of the potential target population relative to the capacity and funding of program implementers, the selection of EBIs that maximize program effects while minimizing costs, and the ability of program implementers to leverage the resources of other public and nonpublic health organizations to facilitate implementation.
Joseph DA, DeGroff A. The CDC Colorectal Cancer Control Program, 2009-2015. Prev Chronic Dis. 2019 Dec 5;16:E159. doi: 10.5888/pcd16.190336. PMID: 31808418; PMCID: PMC6896829.
Another explanation is that some EBIs and SAs can be integrated into clinical practice through clinics’ electronic health records systems. For example, by using data from electronic health records, patient reminder letters can be generated and personalized with each patient’s name and address, preferred language, the name of the patient’s primary care provider, and their history of CRC screening (eg, type and time of most recent test). Although it takes resources to program electronic health records and to set up these strategies initially, clinic health information technology and automated calling and texting systems can support implementation.[[27,28]]
Maxwell AE, DeGroff A, Hohl SD, Sharma KP, Sun J, Escoffery C, Hannon PA. Evaluating Uptake of Evidence-Based Interventions in 355 Clinics Partnering With the Colorectal Cancer Control Program, 2015-2018. Prev Chronic Dis. 2022 May 19;19:E26. doi: 10.5888/pcd19.210258. PMID: 35588522; PMCID: PMC9165474.
Team-based care delivery models also supported sustainability. Team-based care has been shown to improve efficiency, effectiveness, value of care, and patient and provider experiences (Jesmin et al., 2012; Schottenfeld et al., 2016).
Schlueter D, DeGroff A, Soloe C, Arena L, Melillo S, Tangka F, Hoover S, Subramanian S. Factors That Support Sustainability of Health Systems Change to Increase Colorectal Cancer Screening in Primary Care Clinics: A Longitudinal Qualitative Study. Health Promot Pract. 2023 Jul;24(4):755-763. doi: 10.1177/15248399221091999. Epub 2022 May 18. PMID: 35582930; PMCID: PMC9672135.
Respondents noted the importance of planning for sustainability from initiation of CRCCP implementation by allocating funding to integrate EBIs into FQHC practices. Respondents reported that FQHCs were encouraged to apply funding in ways that directly supported sustainability, such as building infrastructure and long-term FQHC practices (e.g., EHR assessments, quality improvement [QI] efforts, and workflow adaptations) versus funding staff positions (e.g., patient navigators) requiring new funding sources once CRCCP funding ends.
Schlueter D, DeGroff A, Soloe C, Arena L, Melillo S, Tangka F, Hoover S, Subramanian S. Factors That Support Sustainability of Health Systems Change to Increase Colorectal Cancer Screening in Primary Care Clinics: A Longitudinal Qualitative Study. Health Promot Pract. 2023 Jul;24(4):755-763. doi: 10.1177/15248399221091999. Epub 2022 May 18. PMID: 35582930; PMCID: PMC9672135.
A key theme across all awardees was the essential nature of coordinating EBIs and SAs with existing FQHC practices to expand reach of clinics’ prevention efforts and increase efficiency.
Schlueter D, DeGroff A, Soloe C, Arena L, Melillo S, Tangka F, Hoover S, Subramanian S. Factors That Support Sustainability of Health Systems Change to Increase Colorectal Cancer Screening in Primary Care Clinics: A Longitudinal Qualitative Study. Health Promot Pract. 2023 Jul;24(4):755-763. doi: 10.1177/15248399221091999. Epub 2022 May 18. PMID: 35582930; PMCID: PMC9672135.
Programmatically, because EBIs can be resource-intensive to implement irrespective of the clinic size, our results support targeting larger clinics, when feasible and appropriate, where greater impact can be achieved.
Sharma KP, DeGroff A, Scott L, Shrestha S, Melillo S, Sabatino SA. Correlates of colorectal cancer screening rates in primary care clinics serving low income, medically underserved populations. Prev Med. 2019 Sep;126:105774. doi: 10.1016/j.ypmed.2019.105774. Epub 2019 Jul 15. PMID: 31319118; PMCID: PMC6904949.
EHR systems, a reservoir of patient information, were also found to be an important component of information sharing to support integrated implementation. Although investing in functional EHR systems can be costly, these systems are recognized as essential to enable optimal, integrated, patient-centered care because they allow for the abstraction of accurate clinical information.
Soloe C, Arena L, Schlueter D, Melillo S, DeGroff A, Tangka F, Hoover S, Subramanian S. Factors that support readiness to implement integrated evidence-based practice to increase cancer screening. Implement Sci Commun. 2022 Oct 6;3(1):106. doi: 10.1186/s43058-022-00347-6. PMID: 36199117; PMCID: PMC9535984.
The indirect overarching component (which is included in the total non-clinical cost) was about $475–$793 per person served for both types of programs. These costs are likely to decrease if programs expand to cover a large cohort of individuals as economies of scale are achieved.
Subramanian S, Tangka FKL, Hoover S, Royalty J, DeGroff A, Joseph D. Costs of colorectal cancer screening provision in CDC's Colorectal Cancer Control Program: Comparisons of colonoscopy and FOBT/FIT based screening. Eval Program Plann. 2017 Jun;62:73-80. doi: 10.1016/j.evalprogplan.2017.02.007. Epub 2017 Feb 7. PMID: 28190597; PMCID: PMC5863533.
The total number of people screened had some effect on the direct clinical cost per person; programs with large populations screened had $292 lower costs than programs with small populations screened.
Subramanian S, Tangka FKL, Hoover S, Cole-Beebe M, Joseph D, DeGroff A. Comparison of Program Resources Required for Colonoscopy and Fecal Screening: Findings From 5 Years of the Colorectal Cancer Control Program. Prev Chronic Dis. 2019 Apr 25;16:E50. doi: 10.5888/pcd16.180338. PMID: 31022371; PMCID: PMC6513474.
Our findings expand on our prior analysis and use 5 years of data to quantify the presence of economies of scale — programs that screen a larger number of people had lower cost per person than programs that screen a smaller number of people.
Subramanian S, Tangka FKL, Hoover S, Cole-Beebe M, Joseph D, DeGroff A. Comparison of Program Resources Required for Colonoscopy and Fecal Screening: Findings From 5 Years of the Colorectal Cancer Control Program. Prev Chronic Dis. 2019 Apr 25;16:E50. doi: 10.5888/pcd16.180338. PMID: 31022371; PMCID: PMC6513474.
Our analysis of the activity-based cost data across 5 years of the CRCCP reveals potential economies of scale: programs with larger screening volume incurred a lower cost per person served than smaller-volume programs. Therefore, encouraging partnerships to foster large-scale programs could be more efficient than funding multiple small screening programs.
Subramanian S, Tangka FKL, Hoover S, Cole-Beebe M, Joseph D, DeGroff A. Comparison of Program Resources Required for Colonoscopy and Fecal Screening: Findings From 5 Years of the Colorectal Cancer Control Program. Prev Chronic Dis. 2019 Apr 25;16:E50. doi: 10.5888/pcd16.180338. PMID: 31022371; PMCID: PMC6513474.
In general, the cost per person screened at FQHCs participating in our study tended to be lowest in those with large target populations. All interventions have fixed implementation costs; therefore, the greater the number of persons screened because of the intervention, the lower the cost per person screened.
Subramanian S, Tangka FKL, Hoover S. Role of an Implementation Economics Analysis in Providing the Evidence Base for Increasing Colorectal Cancer Screening. Prev Chronic Dis. 2020 Jun 25;17:E46. doi: 10.5888/pcd17.190407. PMID: 32584756; PMCID: PMC7316416.
In addition, prior studies of cancer programs have shown that these programmatic costs have significant economies of scale and, as program increase in size, the programmatic cost per person serves decreases substantially (Subramanian, Ekwueme, Gardner, Bapat, & Kramer, 2008; Trogdon, Ekwueme, Subramanian, & Crouse, 2014).
Tangka FKL, Subramanian S, Hoover S, Royalty J, Joseph K, DeGroff A, Joseph D, Chattopadhyay S. Costs of promoting cancer screening: Evidence from CDC's Colorectal Cancer Control Program (CRCCP). Eval Program Plann. 2017 Jun;62:67-72. doi: 10.1016/j.evalprogplan.2016.12.008. Epub 2016 Dec 12. PMID: 27989647; PMCID: PMC5840873.
As in previous evaluations of the cost of cancer screening programs,[[11, 12]] there appears to be some economies of scale associated with the cost of implementing the interventions. Specifically, Health Systems with larger numbers of patients were likely able to distribute fixed costs associated with the interventions across more patients. In other words, the interventions are effective in all settings but may be more costly to implement in smaller clinics based on their number of patients.
Tangka FKL, Subramanian S, Hoover S, Lara C, Eastman C, Glaze B, Conn ME, DeGroff A, Wong FL, Richardson LC. Identifying optimal approaches to scale up colorectal cancer screening: an overview of the centers for disease control and prevention (CDC)'s learning laboratory. Cancer Causes Control. 2019 Feb;30(2):169-175. doi: 10.1007/s10552-018-1109-x. Epub 2018 Dec 14. PMID: 30552592; PMCID: PMC6382575.
Additionally, given that these are rural FQHCs serving small populations (all but one FQHC provided FIT kits to less than 1,000 patients during the study), we would anticipate that their costs would be generally higher than high-volume centers, as they are unable to reap benefits from economies of scale (Subramanian et al., 2017; Trogdon et al., 2014)
Conn ME, Kennedy-Rea S, Subramanian S, Baus A, Hoover S, Cunningham C, Tangka FKL. Cost and Effectiveness of Reminders to Promote Colorectal Cancer Screening Uptake in Rural Federally Qualified Health Centers in West Virginia. Health Promot Pract. 2020 Nov;21(6):891-897. doi: 10.1177/1524839920954164. Epub 2020 Sep 29. PMID: 32990048; PMCID: PMC7894066.